Bispecific Antibodies: What They Are and Their Applications
In this Article
All of the products listed in AAA Biotech’s catalog are strictly for research-use only (RUO).

Key Takeaways
- Bispecific antibodies enable a single molecule to bind two different targets at once (compared to a traditional antibody that can only bind two of the same targets).
- BsAbs come in various formats, including fully intact antibodies (e.g., using "knobs-into-holes" engineering) and smaller, fragment-based forms.
- Producing BsAbs is complex due to the risk of "mispaired" chains, which can lead to low yields of the desired product.
- Production cost for BsAbs tends to be on the expensive side.
Bispecific antibodies (BsAbs) were engineered to tackle the complexity of targeting two different epitopes at the same time by combining the binding regions of two different antibodies into a single molecule. This was (and still is) something not possible to produce with a conventional antibody.
The following sections will discuss bispecific antibodies in detail, how they work, how they differ from more traditional forms of antibodies, and the various applications and challenges of this emerging technology.
NOTE: If you want to learn more about antibodies in general, check our guide on what antibodies are.
How Do Bispecific Antibodies Work?
If the bispecific antibody is functioning correctly, it can bring cells into contact, neutralize multiple targets/signals at once, or stabilize multi-component biological processes, depending on the design of the individual bispecific antibody.
However, it should be noted that the mechanisms of action of a bispecific antibody depend almost entirely on which two targets it is designed to bind.
With that said, there are some fundamental ways that BsAbs exert their effects:
Recruiting Immune Cells to a Target:
One powerful use of bispecifics is to bridge immune cells to diseased cells, thereby directing an immune attack. This physically draws the T cell into close proximity to the diseased cell, enabling the T cell to release perforin, granzymes, and other cytotoxic molecules to kill the diseased cell.
Beyond just T cells, other bispecific designs can similarly recruit natural killer (NK) cells or other immune effectors and lead them directly to tumor cells in order to provoke targeted destruction of the cell.
Dual-Pathway Blockade
Another strategy is to block two molecular targets or signaling pathways at once on the same cell or within the same disease process/pathway. Many diseases (especially cancers) are adept at using alternate pathways to escape the effect of a single-target drug. A bispecific antibody can be crafted to hit two pro-disease signals simultaneously, reducing the chance of such escape.
Forcing Protein Complexes
Bispecifics can also be used to bring together two proteins that need to interact as part of a therapeutic effect.
How Are Bispecific Antibodies Made?
Manufacturing a bispecific antibody is more complex than making a conventional monoclonal antibody, primarily due to the chain association issue. In this, four chains (two heavies, two lights) can mis-pair in many incorrect combinations.
With that said, thanks to rapid progress in protein engineering and bioprocessing, scientists have developed several strategies that allow for the reliable creation of bispecific antibodies:
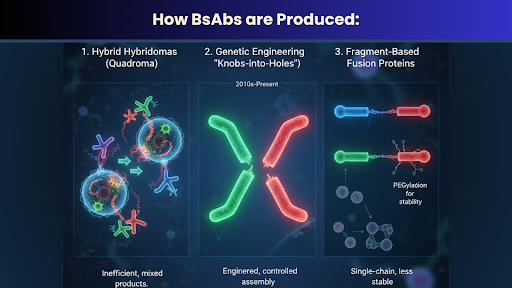
Hybrid Hybridomas (Quadroma Method): In early experiments, researchers fused two different antibody-producing hybridoma cells to create a single “quadroma” cell that secretes two distinct heavy chains and two distinct light chains. However, the method yields a variety of products (including undesirable heavy-chain homodimers and mis-paired light chains), and only a small fraction of the antibodies actually wind up being the desired bispecific.
While this approach was used in the creation of one of the first bispecific antibodies (catumaxomab, approved in 2009), it is rarely used today due to its inefficiency and the developments of subsequent techniques.
Genetic Engineering (“Knobs-into-Holes”): Modern bispecific antibodies often rely on recombinant DNA engineering to preferentially assemble the correct antibody pairs. One elegant solution involves engineering the Fc region of the antibody heavy chains so that one heavy chain has a protruding “knob” amino acid mutation and the other has a complementary “hole”. This knobs-into-holes design encourages the two different heavy chains to heterodimerize with each other (fitting like a puzzle piece) instead of homodimerizing.
Fragment-Based Fusion Proteins: Not all bispecifics are full-size IgG antibodies. Many are smaller, antibody-fragment, constructs that fuse two single-chain variable fragments (scFvs) or other binding domains into one protein. These fragment-based bispecifics are typically produced in microbial expression systems (like E. coli) since they don’t require the complex folding of an Fc region. An advantage of this approach is that it sidesteps the heavy/light chain pairing problem entirely (the molecule is encoded by a single gene, yielding a single-chain protein). However, a drawback is that without an Fc region, these constructs lack the stability and long half-life of full antibodies. As a result, they often have short plasma half-lives, meaning they may need continuous infusion or additional modifications (such as PEGylation or albumin-binding domains) to remain in circulation.
What Is the Difference Between Monoclonal and Bispecific Antibodies?
Monoclonal antibodies (mAbs) and bispecific antibodies are both antibodies, but they differ fundamentally in their specificity and structure. A monoclonal antibody comes from a single clone of B cells, so every antibody molecule is identical and monospecific – meaning both of its arms bind to the same antigen (the same epitope). In other words, a standard mAb has two identical binding sites that can only recognize the same exact target epitope. By contrast, a bispecific antibody is engineered to have two different binding domains within one molecule, so its two arms can bind two different targets. Functionally, this makes a bispecific akin to having two separate antibodies in one. One arm might latch onto antigen X while the other grabs antigen Y.
Are Bispecific Antibodies Considered An Immunotherapy?
In many cases, yes, bispecific antibodies (especially those used in cancer drugs) are considered a form of immunotherapy. Immunotherapy refers to treatments that harness or direct the patient’s immune system itself to fight disease. Many bispecific antibodies fall squarely in this category because they deliberately engage immune cells as part of their actual mechanism of action. For example, any bispecific that interacts with a T-cell that brings it/them into contact with cancer cells is activating the immune system to kill tumors, which is the essence of immunotherapy. The Cancer Research Institute classifies bispecific antibodies as a new type of antibody-based immunotherapy, also specifically noting that by combining the targeting regions of two antibodies, bispecifics can bind to a tumor cell and an immune cell simultaneously.
What Are the Problems with Bispecific Antibodies?
Despite their potential, bispecific antibodies do come with specific drawbacks that researchers and clinicians need to grapple with. Some of these include:
Manufacturing Complexity: The first challenge is production, as producing a bispecific antibody is significantly more complex than producing a traditional mAb. When a cell is engineered to make two different heavy chains and two different light chains, a variety of mis-paired combinations can result. This complexity can, and very often does, increase production costs and development time. Every new bispecific format might require a tailored manufacturing and quality control process, which is much more labor/material-intensive than the well-established platform processes for “ordinary” mAbs.
Stability and Half-Life Issues: Many bispecific formats, particularly those that lack the stabilizing Fc region, have short in-vivo half-lives. While a short half-life can be partly mitigated by strategies like continual infusion or adding half-life extension domains, it still remains a very real drawback compared to conventional antibodies that can be administered weekly or monthly.
Immune-Related Side Effects: Bispecific antibodies that engage immune cells have the potential to be extremely potent, and this heightened activity comes with a risk of very serious side effects. Two of the more notorious ones being Cytokine Release Syndrome (CRS) and neurotoxicity. CRS is an intense systemic inflammatory response caused by the overactivation of immune cells, releasing cytokines, leading to fever, hypotension, and organ dysfunction.
Expensive: Bispecific antibodies are expensive to develop and manufacture, which often translates to higher costs for therapies involving them. Some of the approved BsAbs are priced in the hundreds of thousands of dollars for a course of treatment. This is in direct contrast to polyclonal antibodies, which are significantly cheaper due to their simple production methodology/process.
Regulatory and Development Hurdles: Developing a bispecific antibody can pose additional hurdles in clinical research and regulatory approval. For one, the complexity of the molecule means that regulators expect a robust demonstration that the product is consistent and well-characterized (which, given multiple binding sites and possible variants, is not trivial). Explaining the mechanism of action for a bispecific may also be more involved, since, essentially, you have to validate two targets and the rationale for using both.
Final Words
Ultimately, bispecific antibodies are a next-generation technology that tackles the main limitation of conventional mAbs. Although they are expensive to produce and do come with their own set of new challenges, it is only a matter of time before researchers are able address these one-by-one once these antibodies are able to be produced in a cost-effective manner.
If you’re looking for high-affinity antibodies for research, choose AAA Biotech. Products include phospho antibodies, recombinant antibodies, and more.
Faq's
What are bispecific antibodies?
Bispecific antibodies (BsAbs) are proteins engineered to bind to two different antigens or epitopes at the same time. These were designed to overcome the limitations posed by monoclonal antibodies (which are monospecific).
What's the main difference between a bispecific and a monoclonal antibody?
A monoclonal antibody (mAb) has two identical binding arms that target a single antigen, whereas a bispecific antibody is engineered with two distinct binding arms, allowing it to bind to two different targets simultaneously. This is like having two different drugs combined into one molecule.
Can they be personalized for each patient?
Although it is still a very emerging technology, per existing research and trials, it cannot be explicitly personalized.
What are the major research challenges in developing BsAbs?
The primary challenges include manufacturing complexity due to the need to assemble two different antibody halves correctly. Incorrect assembly can lead to mis-paired products that are non-functional or function in unintended ways. Researchers are also working to improve the stability and half-life of smaller, fragment-based, BsAbs.