Monoclonal Antibody Production: Process, Methods, and Applications
In this Article
- The Evolution of Antibody Engineering: From Serum to Sequence
- How are Monoclonal Antibodies Produced? Primary Methods
- Upstream Processing: From Clone to Bioreactor
- Downstream Processing: The Science of Purification
- Applications: How mAbs are Reshaping Medicine in 2026
- AAA Biotech: Your Partner in Protein Research
All of the products listed in AAA Biotech’s catalog are strictly for research-use only (RUO).

Summary:
Monoclonal antibodies (mAbs) drive modern medicine through precise immune engineering. Key production methods include hybridoma technology (animal-based fusion), phage display (in vitro screening), and single B-cell sequencing (high-affinity isolation). Manufacturing uses CHO/HEK293 cells in fed-batch/perfusion bioreactors, followed by Protein A purification, virus inactivation, and polishing. Applications span oncology (e.g., Keytruda, ADCs), autoimmune diseases, infections, and Alzheimer’s.
The biological revolution of the 21st century is defined largely by our ability to harness the immune system’s own machinery to create precision-engineered medicines. At the center of this revolution are monoclonal antibodies (mAbs) - highly specific proteins that can be tailored to bind to virtually any biological target.
The journey from an initial concept to a validated therapeutic or research reagent involves a complex blend of immunology, genetic engineering, and advanced bioprocessing.
For researchers and clinicians, understanding how monoclonal antibodies are produced, formed, and made is essential for advancing everything from basic proteomics to life-saving oncology treatments.
The Evolution of Antibody Engineering: From Serum to Sequence
The history of antibody production is a transition from the broad, natural defenses of the body to the precision of molecular engineering. Historically, researchers relied on polyclonal antibodies (pAbs), which are derived from multiple B-cell clones and recognize a diverse array of epitopes on a single antigen.
The breakthrough came in 1975 when Georges Köhler and César Milstein developed the hybridoma technique.
Today, the field is dominated by recombinant DNA technology, where the specific sequences encoding the antibody are inserted into high-efficiency mammalian host cells, such as Chinese Hamster Ovary (CHO) or Human Embryonic Kidney (HEK293) cells, for large-scale manufacturing.
To understand mAbs in-depth, please refer to: What Are Monoclonal Antibodies (mAbs): Their Uses, Types & Benefits
How are Monoclonal Antibodies Produced? Primary Methods
The development of monoclonal antibodies is a multi-stage process that begins with discovery and ends with scalable manufacturing. There are 3 principal methodologies used by industry leaders to generate these high-value molecules: hybridoma technology, phage display, and single B-cell sequencing.
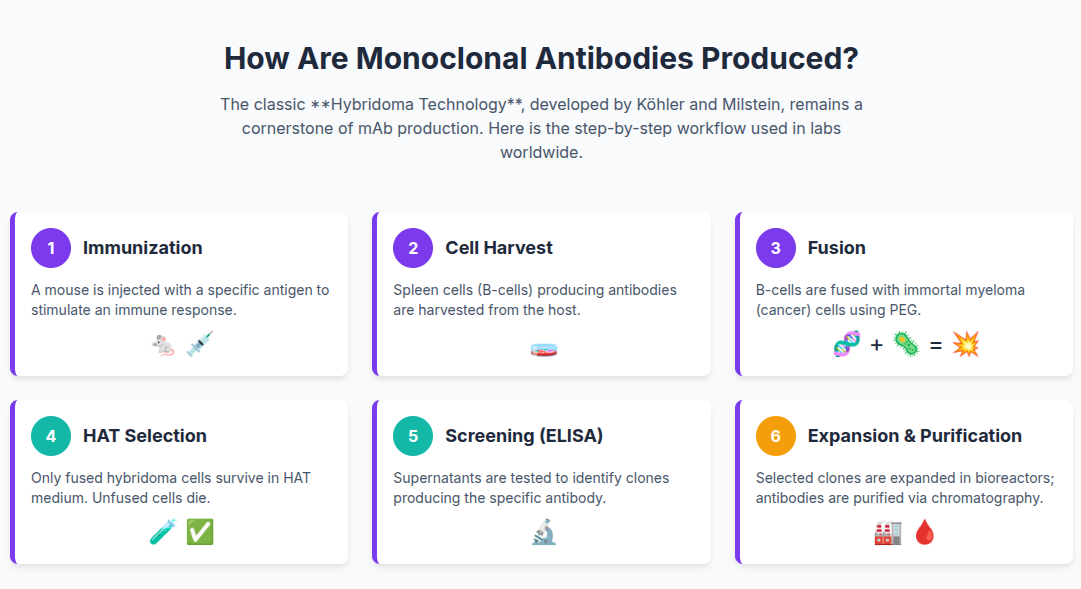
Hybridoma Technology: The Classical Approach
Hybridoma technology remains a cornerstone for producing highly sensitive binders. The process follows a well-defined sequence of biological events:
- Immunization: A host animal (typically a mouse) is injected
with the target antigen to stimulate B-cell production.
- Cell Fusion: Once a sufficient titer is reached, the spleen
is removed, and the B-cells are fused with immortal myeloma cells using
polyethylene glycol (PEG) or electrofusion.
- Selection: The resulting mixture is cultured in HAT
(Hypoxanthine-Aminopterin-Thymidine) medium, which allows only the successfully
fused hybridoma cells to survive.
- Cloning and Screening: Individual hybridoma cells are
separated through limiting dilution and screened via ELISA to identify the
specific clones that produce the desired antibody.
While hybridomas offer the benefit of natural in-vivo affinity maturation - meaning the animal's body has already optimized the antibody’s binding strength - the process is time-consuming, taking up to 12 weeks. Furthermore, because the antibodies are murine, they often require "humanization" to be used as human therapeutics, which involves grafting the mouse binding regions onto a human antibody framework.
Phage Display: In Vitro Innovation
Phage display technology is a molecular approach that bypasses animal immunization. In this method, antibody gene libraries are inserted into bacteriophages so that the antibody fragments are displayed on the phage surface.
- Biopanning: The library is screened against an immobilized
antigen. Only the phages displaying antibodies that bind the antigen are
retained, while the rest are washed away.
- Amplification: The bound phages are eluted and used to
infect E. coli for rapid multiplication.
- Selection Rounds: This process is repeated 2–3 times with
increasing stringency to isolate the highest-affinity binders.
Phage display is significantly faster than hybridoma technology, with timelines of 3–6 weeks. It allows for the use of fully human libraries from the start, eliminating the need for downstream humanization. Additionally, it can identify antibodies against toxic or non-immunogenic antigens that would fail in an animal-based system.
Single B-Cell Sequencing: The New Frontier
Single B-cell sorting and sequencing represent the cutting edge of antibody development. This platform, such as the Native™ Antibody Discovery Platform, uses high-throughput technologies like Fluorescence-Activated Cell Sorting (FACS) or microfluidics to isolate individual antigen-specific B-cells directly from human donors or immunized animals.
- Natural Pairing: Unlike phage display, which often randomly
pairs heavy and light antibody chains, single B-cell methods preserve the
natural cognate pairing found in the original cell, leading to better solubility
and biophysical stability.
- Speed: Selection can take as little as 2–3 weeks
post-immunization.
- Affinity: By tapping into the results of in vivo affinity
maturation, this method yields antibodies with extremely high specificity and
affinity.
Upstream Processing: From Clone to Bioreactor
Once a specific clone or sequence has been identified, it must be produced in large quantities. This is known as upstream processing, and it revolves around the cultivation of mammalian cells in controlled environments.
Host Cell Selection: CHO vs. HEK293
The choice of the production host is a critical decision that affects the final product's quality, particularly its post-translational modifications (PTMs) like glycosylation.
- Chinese Hamster Ovary (CHO) Cells: CHO cells are the
industry workhorse, producing over 70% of currently approved biotherapeutics.
They are genetically stable, grow well in suspension at high densities, and are
capable of human-like PTMs. They have a proven safety record and a predictable
regulatory path.
- Human Embryonic Kidney (HEK293) Cells: HEK293 cells are often used for rapid, small-scale production (transient expression) or for specific proteins that require PTMs that CHO cells cannot provide, such as γ-carboxylation. Because they are human cells, they offer the closest possible profile to natural human proteins but carry a higher risk of propagating human-specific viruses, requiring stricter biosafety protocols.
Optimizing the Bioreactor Environment
Upstream processing requires meticulous control over the bioreactor environment to ensure cell health and high antibody titers. Parameters such as dissolved oxygen, pH, temperature, and nutrient concentrations must be monitored in real-time. Modern facilities are moving away from traditional batch processing toward fed-batch and continuous (perfusion) processing.
- Fed-Batch: Nutrients are added periodically to extend the
life of the culture, typically reaching titers of 5–10 g/L.
- Perfusion (Continuous): Fresh media is constantly added
while the product is constantly removed. This achieves significantly higher cell
densities (50–100 million cells/mL) and can reduce manufacturing costs by up to
35% at certain scales.
Downstream Processing: The Science of Purification
After the antibodies are produced in the bioreactor, they are mixed with a complex "soup" of cells, cell debris, and media components. Downstream processing is the multi-step journey to isolate the pure antibody.
1. Clarification and Harvest
The first step is the removal of the cells. This is typically achieved through centrifugation or depth filtration to yield a clarified supernatant known as harvested cell culture fluid (HCCF).
2. Capture Chromatography
The core of the purification process is Protein A affinity chromatography. Protein A is a bacterial protein that binds specifically to the Fc (tail) region of the antibody. This step provides a high degree of purity (often >95%) in a single cycle. The antibodies are eluted from the Protein A resin by lowering the pH, which also helps in the next step: virus inactivation.
3. Virus Inactivation and Filtration
Safety is paramount in mAb production. The low-pH elution from the Protein A step is held for a set period to inactivate enveloped viruses. Later in the process, specialized virus filters (nanofilters) are used to physically remove any remaining viral particles.
4. Polishing Steps
To remove trace impurities like host cell DNA, proteins, and antibody aggregates, "polishing" chromatography is used. This usually involves Anion Exchange (AIEX) and Cation Exchange (CIEX) chromatography, often run in "flow-through" mode, where the impurities stick to the column while the pure antibody passes through.
5. Formulation and Fill-Finish
The final step is ultrafiltration and diafiltration (UF/DF) to concentrate the antibody and exchange the buffer for the final formulation. The product is then filled into sterile vials and packaged for distribution.
Summary:
| Stage | Process | Primary Purpose |
|---|---|---|
| Harvest | Centrifugation / Depth Filtration | Removal of cells and debris |
| Capture | Protein A Chromatography | High-purity isolation of mAb |
| Inactivation | Low-pH Treatment | Inactivation of enveloped viruses |
| Polishing | IEX, HIC, or Mixed-Mode | Removal of trace impurities and aggregates |
| Filtration | Virus Filtration (Nanofiltration) | Removal of viral particles by size |
| Concentration | UF/DF | Buffer exchange and final formulation |
Standard Downstream Workflow
Applications: How mAbs are Reshaping Medicine in 2026
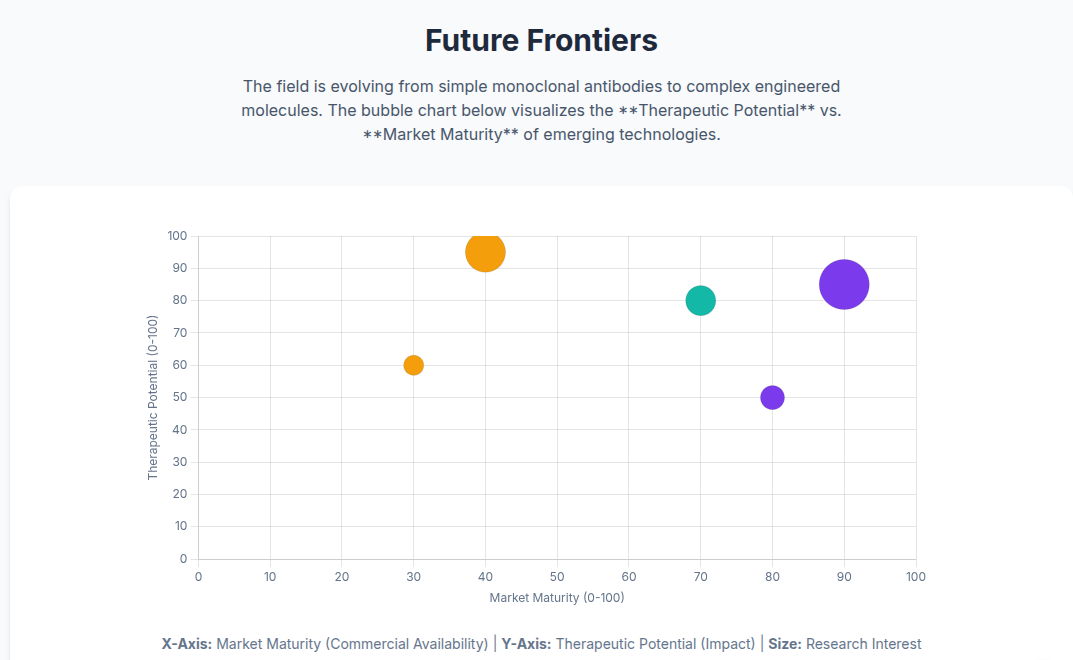
The therapeutic potential of monoclonal antibodies has expanded far beyond simple blocking of receptors. We are now in the era of "non-canonical" antibody formats.
1. Oncology and Targeted Therapy
mAbs like Pembrolizumab (Keytruda) have revolutionized cancer treatment by inhibiting immune checkpoints, allowing the body's own T-cells to attack tumors. In 2026, oncology remains the largest segment of the mAb market.
2. Antibody-Drug Conjugates (ADCs)
ADCs are essentially "guided missiles." They combine a mAb (the guidance system) with a potent cytotoxic drug (the warhead) via a stable linker. This allows the drug to be delivered directly to the cancer cell, minimizing damage to healthy tissue. Currently, over 19 ADCs are FDA-approved, with hundreds more in the pipeline.
3. Bispecific Antibodies (bsAbs)
Bispecific antibodies can bind to two different targets at once. For example, one arm might bind to a cancer cell while the other binds to a T-cell, physically bringing them together to trigger an immune attack. These are increasingly used in liquid and solid tumors, as well as autoimmune diseases.
4. Autoimmune and Infectious Diseases
mAbs are used to treat rheumatoid arthritis, Crohn's disease, and psoriasis by neutralizing pro-inflammatory cytokines like TNF-α, or IL-17A. They also provide passive immunity against infectious agents like SARS-CoV-2 or RSV for immunocompromised patients.
5. Neurological Disorders
Emerging mAbs like Lecanemab and Donanemab target amyloid-beta plaques in the brain, offering the first effective treatments to slow cognitive decline in Alzheimer’s disease.
AAA Biotech: Your Partner in Protein Research
AAA Biotech (AAABio) is a "one-stop shop" for high-quality protein research tools, serving the global scientific community for over 10 years. Based in San Diego, the company is dedicated to providing validated reagents that researchers can trust for precise outcomes.
Specific Strengths and Services:
- Validated Reagents: AAA Biotech’s catalog includes
thousands of monoclonal and polyclonal antibodies, ELISA kits, and recombinant
proteins.
- Rigorous Validation: Antibodies are tested in-house for a
wide range of applications, including Western Blot (WB), IHC, ELISA, Flow
Cytometry (FC), and Immunoprecipitation (IP).
- Rare Species Coverage: AAA Biotech specializes in reagents
for both common and hard-to-find species and targets.
- Recombinant Excellence: The company offers a robust
selection of recombinant proteins with >90% purity, available in multiple tags
like FLAG, GST, and His.
- Custom Development: AAA Biotech is always open to
collaborating with customers to develop unique products that meet specific
experimental models.
By combining deep scientific expertise with a commitment to customer success, we ensure that scientists have the tools they need to propel vital research forward, leading to the next generation of therapies and diagnostics.
Conclusion
The production of monoclonal antibodies has matured from a labor-intensive laboratory curiosity into a sophisticated, high-tech industry. In 2026, the integration of continuous bioprocessing, artificial intelligence, and modular facility design will continue to drive down costs and expand the possibilities of what these molecules can achieve.
Whether it is through the rapid discovery of lead candidates via phage display
or the robust large-scale expression in CHO cells, the goal remains the same: to
produce highly specific, safe, and effective tools for research and medicine.
By understanding how monoclonal antibodies are produced,
formed, and made, the scientific community can better leverage these powerful
tools to tackle the world's most challenging health problems.
Faq's
1. How are monoclonal antibodies produced in simple terms?
Monoclonal antibodies are made by cloning a single type of immune cell that produces exactly one type of antibody. This is usually done by fusing a B-cell (which makes antibodies) with a myeloma cell (which lives forever) to create a "hybridoma" that acts like an antibody factory.
2. Why is CHO cell expression the industry standard?
CHO cells are the "gold standard" because they are robust, can grow in very large quantities, and produce antibodies with glycosylation patterns that are very similar to those found in humans, making the resulting drugs safe and effective.
3. What is the difference between monoclonal and polyclonal production?
Monoclonal production comes from a single cell clone and results in a highly specific, identical antibody. Polyclonal production comes from multiple cell clones and results in a mixture of antibodies that recognize different parts of the same target. Monoclonals are better for therapeutics, while polyclonals are often used for general research.
4. What are the main applications of monoclonal antibodies in 2025-26?
mAbs are used primarily to treat cancer (checkpoint inhibitors, ADCs, Bispecifics), autoimmune diseases (like arthritis and Crohn's), infectious diseases (passive immunity), and neurological disorders like Alzheimer's.
5. How are monoclonal antibodies made to be "fully human"?
"Fully human" antibodies are made using either transgenic mice (mice that have been genetically modified to have human immune systems) or through phage display libraries that use human antibody genes from the start.
6. What are Antibody-Drug Conjugates (ADCs)?
ADCs are a form of targeted therapy where a monoclonal antibody is linked to a potent drug. The antibody finds the cancer cell, and the drug is released inside to kill it, reducing the side effects of traditional chemotherapy.
7. Why are monoclonal antibodies so expensive to develop?
The high cost is due to the complexity of biologics manufacturing, the need for sterile environments, the high cost of raw materials (like Protein A resin), and the rigorous quality control and clinical trials required for regulatory approval.