Understanding The Importance Of Monoclonal Antibodies in Modern Medicine
In this Article
- Structural and Functional Comparison of Monoclonal Antibodies With Polyclonal Antibodies
- Mechanistic Insights: How Monoclonal Antibodies Function
- Therapeutic Applications Across Medical Specialties
- Next-Generation Technologies: ADCs and Bispecifics
- Opinion: The Ethics of Innovation and the Global Access Gap
- Regulatory Outlook: 2025-2026 New Approvals
- Managing Patient Experience and Safety
All of the products listed in AAA Biotech’s catalog are strictly for research-use only (RUO).
Key Takeaways
- Monoclonal antibodies (mAbs) offer precise targeting, unlike polyclonal antibodies’ broad response, enabling reproducible therapies.
- They function via ADCC, CDC, and ADPH, recruiting immune cells to destroy targets.
- Revolutionized oncology with drugs like Keytruda blocking immune checkpoints.
- Lecanemab and Donanemab slow Alzheimer’s by clearing amyloid plaques.
- Effective in infections like RSV via neutralization and prophylaxis.
- Next-gen ADCs and bispecifics deliver payloads and engage T-cells for better efficacy.
- Market tops $210B; biosimilars address global access gaps in LMICs.
- Administered via infusion/injection; monitor for reactions like IRRs.
The medical organizations in the last few decades have seen the transition from broad-spectrum chemical interventions to the surgical precision of biological engineering.
At the vanguard of this shift are monoclonal antibodies (mAbs) - laboratory-engineered proteins that have revolutionized the treatment of previously intractable diseases. The role of monoclonal antibodies in contemporary clinical practice extends far beyond simple symptom management, representing a fundamental change in how clinicians approach oncology, neurology, and chronic inflammatory conditions.
These sophisticated molecules are designed to mimic the human immune system’s natural defenses, yet they possess a level of specificity and reproducibility that natural polyclonal responses cannot match.
Structural and Functional Comparison of Monoclonal Antibodies With Polyclonal Antibodies
The clinical utility of monoclonal antibodies is best understood when compared to polyclonal antibodies. While the human body naturally produces polyclonal antibodies - a mixture of different antibodies targeting multiple sites (epitopes) on a single pathogen, monoclonal antibodies are identical clones derived from a single B-cell lineage.
| Characteristic | Monoclonal Antibodies | Polyclonal Antibodies |
|---|---|---|
| Origin | Derived from a single B-cell clone | Derived from multiple B-cell clones |
| Epitope Specificity | Recognizes a single specific epitope | Recognizes multiple epitopes on one antigen |
| Batch Consistency | Highly reproducible and standardized | Variable; depends on animal host response |
| Binding Affinity | Specific and uniform across all molecules | Average affinity across a diverse population |
| Risk of Cross-Reactivity | Minimal, due to single epitope targeting | Higher, due to heterogeneous binding |
| Primary Clinical Use | Targeted therapy and precision diagnostics | Broad research assays and antivenoms |
Table 01: A Quick Comparison between mAbs and pAbs
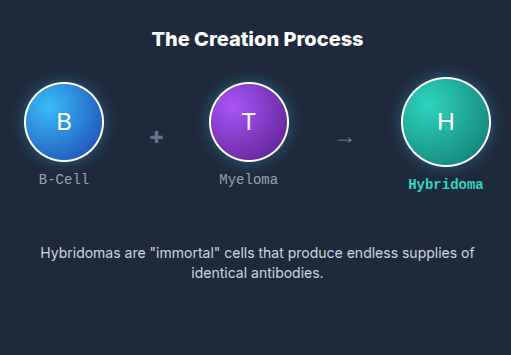
To better understand the structure of monoclonal antibodies, here is an overview of mAb creation:
Mechanistic Insights: How Monoclonal Antibodies Function
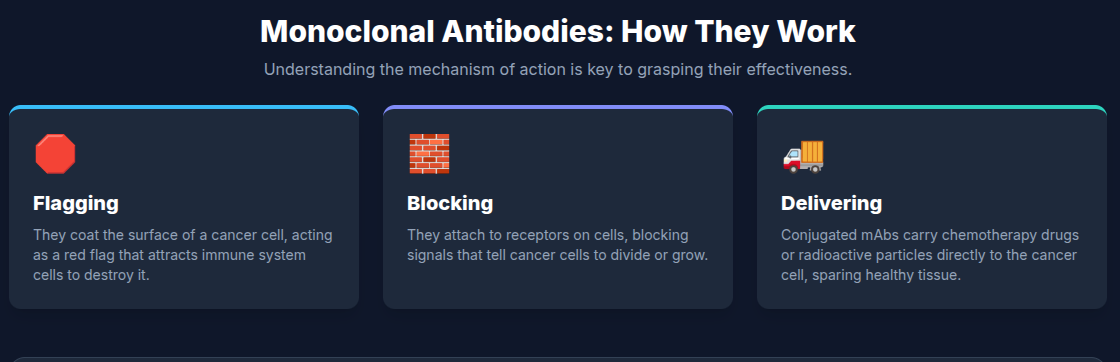
The effectiveness of monoclonal antibody medicine relies on a diverse repertoire of mechanisms of action. These can be broadly categorized into direct mechanisms, where the antibody itself blocks or stimulates a pathway, and indirect mechanisms, where the antibody acts as a beacon for the immune system.
Immune-Mediated Effector Functions
The most potent aspect of monoclonal antibodies for treatment is often their ability to recruit the rest of the immune system. This occurs through several pathways:
- Antibody-Dependent Cellular Cytotoxicity (ADCC): When an antibody binds to a target cell, its Fc region acts as a handle grip for Natural Killer (NK) cells. The NK cell then releases perforins and granzymes to destroy the target.
- Complement-Dependent Cytotoxicity (CDC): The bound antibody can initiate the complement cascade, a series of proteins that form a "membrane attack complex," literally punching holes in the target cell.
- Antibody-Dependent Cellular Phagocytosis (ADPH): Antibodies can coat (opsonize) a pathogen, making it easier for macrophages to engulf and digest it.
Therapeutic Applications Across Medical Specialties
The versatility of monoclonal antibody medicine has allowed it to penetrate almost every field of medicine. While cancer was the initial focus, the landscape has expanded significantly into neurology, infectious disease, and chronic inflammatory disorders.
Oncology: The Transformation of Cancer Care
Monoclonal antibodies are the foundation of modern immuno-oncology. Beyond simple targeting, the introduction of immune checkpoint inhibitors (ICIs) has fundamentally altered the prognosis for metastatic cancers. Drugs like Pembrolizumab (Keytruda) do not target the cancer directly; instead, they block the "off switches" (like PD-1) that tumors use to evade detection by the immune system.
| Generic Name | Target | Indication | Mechanism |
|---|---|---|---|
| Rituximab | CD20 | Non-Hodgkin Lymphoma | Direct lysis, ADCC, CDC |
| Trastuzumab | HER2 | Metastatic Breast Cancer | Inhibition of HER2 signaling |
| Pembrolizumab | PD-1 | Melanoma, NSCLC | Immune Checkpoint Blockade |
| Bevacizumab | VEGF | Colorectal Cancer | Angiogenesis Inhibition |
| Daratumumab | CD38 | Multiple Myeloma | Multi-faceted immune killing |
Table 02: Prominent Monoclonal Antibodies in Clinical Oncology (2025-2026)
Neurology: A New Era for Alzheimer’s Disease
One of the most dramatic developments in the progression of monoclonal antibody therapies occurred in the field of neurology. For decades, Alzheimer’s disease was treated only symptomatically. However, the approval of Lecanemab (Leqembi) and Donanemab (Kisulna) in 2023–2025 has introduced the first truly disease-modifying therapies.
These antibodies are designed to enter the brain and bind to amyloid-beta, the toxic protein that forms plaques in the brains of Alzheimer’s patients. By binding to these plaques, the antibodies facilitate their clearance by microglia, the brain’s resident immune cells. Clinical trials such as Clarity AD and TRAILBLAZER-ALZ have shown that these drugs can slow cognitive decline by approximately 27% to 35% when administered in the early stages of the disease.
Infectious Disease: Beyond the Pandemic
While the role of monoclonal antibodies gained global prominence during the COVID-19 pandemic, their application in infectious diseases is much broader. Monoclonal antibodies are now used for post-exposure prophylaxis in rabies and hepatitis B, and for the prevention of Respiratory Syncytial Virus (RSV) in high-risk infants.
The approval of Clesrovimab in 2025 for the prevention of RSV lower respiratory tract disease in neonates highlights the shift toward using antibodies as a form of "instant vaccine" for vulnerable populations who cannot mount an effective response to traditional immunization.
Next-Generation Technologies: ADCs and Bispecifics
As the field of monoclonal antibody medicine matures, researchers are moving beyond the traditional monospecific IgG format to create multi-functional molecules.
Antibody-Drug Conjugates (ADCs)
ADCs are perhaps the most successful of the "next-gen" formats. They consist of a monoclonal antibody chemically linked to a potent cytotoxic drug. The antibody serves as a delivery vehicle, bringing the "payload" directly to the cancer cell and sparing healthy tissue from the toxic effects of chemotherapy.
Bispecific Antibodies (BsAbs) and T-cell Engagers
Bispecific antibodies are designed with two different binding domains. A common format is the bispecific T-cell engager (BiTE), which binds to a tumor antigen with one arm and to the CD3 receptor on T-cells with the other. This physically bridges the T-cell and the tumor cell, forcing the T-cell to recognize and kill the cancer regardless of whether the cancer is trying to hide.
The market for bispecific antibodies is projected to grow at a CAGR of over 18% through 2035, reaching a valuation of approximately $52 billion. This growth is driven by their superior efficacy in treating hematological malignancies, such as multiple myeloma, where traditional mAbs have sometimes reached a plateau.
Opinion: The Ethics of Innovation and the Global Access Gap
Many researchers in the field believe that we are approaching a critical juncture in the history of monoclonal antibody drugs. We have achieved a level of technical mastery that was unimaginable twenty years ago - we can now design antibodies that enter cells, cross the blood-brain barrier, and deliver lethal toxins with sub-cellular precision. However, this innovation is currently concentrated in a few wealthy markets.
Approximately 80% of the monoclonal antibody market is concentrated in the United States, Europe, and Canada. This means that while patients in North America are gaining access to disease-modifying Alzheimer’s treatments, patients in Africa and Southeast Asia are often unable to access even basic antibodies for cancer or infectious diseases.
The solution lies not just in better science, but in better economics. The industry must prioritize "local" manufacturing in LMICs and support the development of biosimilars. Biosimilars, essentially generic versions of biological drugs, are expected to drive down prices through market competition. In late 2025 and early 2026, we saw a surge in biosimilar approvals for drugs like Denosumab and Ranibizumab, which is a promising step toward a more equitable healthcare landscape.
As a bonus guide, here is the infographic explaining the working of mAbs:
Regulatory Outlook: 2025-2026 New Approvals
The pace of regulatory approval for monoclonal antibodies has not slowed. In the first quarter of 2026, the FDA granted several "Fast Track" and "Breakthrough Therapy" designations, signaling a continued commitment to accelerating access to novel biologics.
| Drug Name | Target | Indication | Status/Date |
|---|---|---|---|
| Garadacimab | Factor XIIa | Hereditary Angioedema | Approved Jan 2025 |
| Nipocalimab | FcRn | Myasthenia Gravis | Approved 2025 |
| Telisotuzumab Vedotin | cMET | NSCLC (Lung Cancer) | Approved 2025 |
| Sevabertinib | HER2 | HER2+ NSCLC | Breakthrough Jan 2026 |
| Gotistobart | CTLA-4 | Squamous NSCLC | Orphan Drug Jan 2026 |
| Zoldonrasib | KRAS G12D | G12D-Mutant NSCLC | Breakthrough Jan 2026 |
Table 03: Significant FDA Approvals and Designations (Late 2025 - Early 2026)
These approvals reflect a broader trend: the "purpose of monoclonal antibodies" is shifting toward treating orphan diseases and specific genetic mutations that were previously considered "undruggable."
Managing Patient Experience and Safety
Despite their precision, monoclonal antibodies are not without risks. Because they are proteins, they must be administered via injection or infusion, as the digestive system would simply break them down if taken as a pill. This leads to the risk of "infusion-related reactions" (IRRs).
Understanding Infusion Reactions
Infusion reactions occur when the body’s immune system responds to the sudden influx of foreign protein. Symptoms can range from mild (rash, fever, chills) to severe (anaphylaxis, cytokine release syndrome). Consequently, monoclonal antibody medicine is typically administered in controlled clinical settings where healthcare providers can monitor patients and intervene if a reaction occurs.
Patient Guidelines for Treatment
For patients receiving these therapies, preparation is key. Most clinicians recommend:
- Pre-medication: Using antihistamines or acetaminophen to reduce the risk of a reaction.
- Monitoring: Staying at the clinic for 30–60 minutes post-infusion to ensure safety.
- Reporting: Immediately notifying a provider of any shortness of breath, racing heart, or swelling.
Final Thoughts
The role of monoclonal antibodies in modern medicine is secure. They have moved from experimental niche products to the highest-grossing category of drugs globally, with the market exceeding $210 billion annually.
The next decade of monoclonal antibody development will be defined by three pillars: Intracellular Targeting, Global Affordability, and AI-Assisted Precision.
AAA Biotech and its peers are now looking at "cell-penetrating" antibodies that can reach targets inside the cytosol, potentially opening up treatments for a vast range of intracellular metabolic disorders. As we refine these molecular keys, the promise of a truly personalized medicine, where a drug is designed for a single patient’s unique genetic profile, is no longer a distant dream but an approaching reality.
Faq's
Q1: What exactly are monoclonal antibodies, and how do they differ from regular drugs?
Monoclonal antibodies are "biologics," meaning they are made in living cells rather than through chemical synthesis. Unlike traditional drugs (like aspirin), which are small molecules, monoclonal antibodies are large, complex proteins designed to target one specific site on a cell, much like a key fits a lock.
Q2: What is the main purpose of monoclonal antibodies in cancer treatment?
In oncology, the role of monoclonal antibodies is to either target and kill cancer cells directly, block the signals they need to grow, or "unmask" them so that the patient's own immune system can find and destroy them.
Q3: Why are monoclonal antibodies often used for autoimmune diseases like rheumatoid arthritis?
In autoimmune diseases, the immune system mistakenly attacks the body’s own tissues. Monoclonal antibodies can be designed to bind to and neutralize the specific inflammatory proteins (like TNF-alpha) that cause this damage, effectively "calming down" the overactive immune response.
Q4: How do monoclonal antibodies work against viruses like COVID-19 or RSV?
These antibodies bind to the "spike" or surface proteins of a virus. By coating the virus, they prevent it from attaching to and entering human cells, effectively neutralizing the infection before it can spread.
Q5: Can monoclonal antibodies be administered at home?
While many require a hospital infusion, a growing number of monoclonal antibody drugs are being formulated for subcutaneous injection. If your doctor determines it is safe, you may be taught to give yourself these shots at home, similar to how an insulin pen is used.
Q6: Are there any long-term risks with monoclonal antibody medicine?
Because some mAbs suppress certain parts of the immune system, there is a risk of increased susceptibility to infections. For specific treatments like those for Alzheimer’s, there is a known risk of brain swelling (ARIA) that requires regular MRI monitoring.
Q7: What is a "biosimilar," and is it as safe as the original antibody?
A biosimilar is a biological product that is highly similar to an FDA-approved "reference" antibody. They undergo rigorous testing to ensure they have no clinically meaningful differences in safety or effectiveness. Biosimilars are crucial for making these expensive treatments more affordable.
Q8: How long does it take for a monoclonal antibody treatment to start working?
This depends on the condition. For infectious diseases, they work almost immediately (passive immunity). For chronic conditions like arthritis or cancer, it may take several weeks or months of regular treatment to see the full therapeutic effect.