A Researcher's Deep Dive into Hybridoma Technology for Monoclonal Antibody Production
In this Article
- Key Takeaways from the Web Blog
- The Core Principle of Hybridoma Technology: Creating Immortality and Specificity
- The Expert Protocol: Production of Monoclonal Antibodies
- Precision Selection: The Molecular Basis of HAT Medium
- Enduring Strengths: Advantages and Application of Hybridoma Technology
- Downstream Excellence: Hybridoma Technology Purification
- Advance in Hybridoma Technology: Modernizing a Classic Platform
- Strategic Comparison: Hybridoma vs. Recombinant Antibody Platforms
All of the products listed in AAA Biotech’s catalog are strictly for research-use only (RUO).

Key Takeaways from the Web Blog
- Hybridoma technology remains the gold standard for generating monoclonal antibodies with unmatched specificity.
- The fusion of B cells (antibody producers) and immortal myeloma cells creates hybridomas capable of indefinite antibody production.
- Selection in HAT medium ensures only hybridomas (immortal and HGPRT-positive) survive.
- Electrofusion boosts fusion efficiency and clone viability over traditional PEG methods.
- Hybridoma-derived mAbs feature authentic affinity maturation, native chain pairing, and natural post-translational modifications.
- Rigorous purification (affinity, exchange, and ultrafiltration steps) ensures high-purity antibodies.
- Advances include microfluidic high-throughput screening, kinetic analysis, and hybridoma sequencing for superior clone selection.
- Genetic sequencing enables recombinant production, enhancing consistency, scalability, and engineering options
Modern biological discovery and therapeutic development fundamentally rely on highly specific reagents that can target single molecular features. This requirement for unequivocal specificity is met by monoclonal antibodies (mAbs).
The gold standard methodology for generating these highly precise tools is hybridoma technology, an innovative platform that resolves the inherent biological conflict between immune specificity and cellular mortality.
The breakthrough that unlocked the era of monoclonal antibodies occurred in 1975 when César Milstein and Georges J. F. Köhler published their seminal paper detailing the production of monoclonal antibodies in continuous cell culture. Their monumental contribution earned them the 1984 Nobel Prize in Physiology or Medicine. The resulting fused cell line, which combined the B cell's function with immortal growth, was later coined a "hybridoma" by Leonard Herzenberg.
While contemporary methods like phage display and single B-cell sorting offer speed, the biologically vetted specificity provided by the initial hybridoma technology remains irreplaceable for many challenging targets. Understanding the hybridoma technology foundation and its historical context is essential to appreciating the value of robust hybridoma and monoclonal antibodies generated through this method.
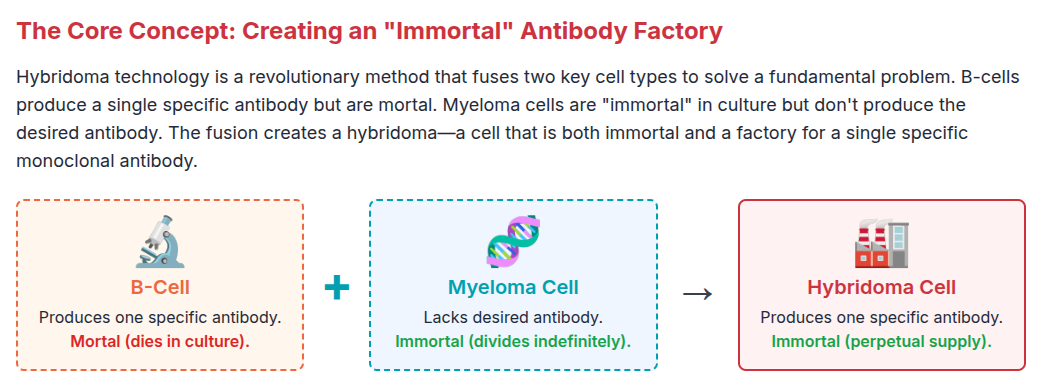
The Core Principle of Hybridoma Technology: Creating Immortality and Specificity
Understanding what hybridoma technology is begins with grasping the molecular
rationale behind the engineered cell fusion. The principle of hybridoma
technology involves fusing two disparate cell lines, thereby complementing the
deficiencies of each parent cell to create an immortal, antibody-secreting
hybrid.
The Complementary Parental Cells
The hybridoma represents a biological chimera engineered to overcome the inherent limits of its parents by combining specific strengths.
Antibody-Producing B Cells (Splenocytes)
- Strength: These cells possess the genetic machinery
required to produce high-affinity antibodies specific to the target antigen
following animal immunization.
- Weakness: B cells are primary cells that are finite and
cannot proliferate indefinitely in standard cell culture conditions.
- Biochemical Status: Functionally, they possess the enzyme
Hypoxanthine-Guanine Phosphoribosyl Transferase (HGPRT), enabling them to
utilize the salvage pathway for nucleotide synthesis.
Immortal Myeloma Cells (Cancerous Plasma Cells)
- Strength: These established cell lines (e.g., SP2/0)
provide indefinite replicative capacity, ensuring continuous culture.
- Weakness: Myeloma cells do not secrete the desired
antibodies and, critically, are deficient in key metabolic enzymes.
- Biochemical Status: They lack the functional HGPRT enzyme
(HGPRT-deficient).
The Fusion Event
The physical fusion, often achieved using chemical “fusogens” like Polyethylene Glycol (PEG) or through electrical discharge (Electrofusion), merges the B cell and myeloma cell.
The resulting hybrid cell, the hybridoma, simultaneously inherits the immortality from the myeloma cell and the HGPRT functionality and target-specific antibody secretion from the B cell.
This fusion generates the hybridoma monoclonal antibody - a pool of identical immunoglobulins secreted by the clonal hybrid cell line.
The Expert Protocol: Production of Monoclonal Antibodies
The successful production of monoclonal antibodies by this method requires meticulous execution across several stages, collectively forming the typical hybridoma technology protocol. This methodology defines the critical steps in hybridoma technology that transition from an immune response in an animal to a stable cell line.
A. Pre-Fusion Stage: Immunization and Preparation
- Antigen Preparation and Immunization: The process begins
with meticulous antigen design and preparation, often involving emulsifying the
antigen with adjuvants (like Freund's adjuvant) to elicit a potent immune
response in the host animal, typically mice.
- Immunization Cycle: Animals are subjected to multiple
injections over a defined timeline (e.g., injections on different
durations - Day 0, Day 21, and a final boost around Day 42) to
optimize B cell maturation and affinity.
- Response Monitoring: Serum screening, typically via Enzyme-Linked Immunosorbent Assay (ELISA), monitors the antibody titer. The "best responder" mouse, which exhibits the strongest specific antibody concentration, is selected as the donor for the spleen.
B. Cell Isolation and Advanced Fusion
The spleen, rich in antibody-producing plasma and memory B cells, is harvested from the best responder. These B cells (splenocytes) are then mixed with prepared, HGPRT-deficient myeloma cells, often at a ratio favoring splenocytes (e.g., 1:1 to 1:5).
While PEG fusion has traditionally been used, advanced protocols increasingly favor Electrofusion to maximize viable clone yield. The decision to use superior fusion methods is crucial because higher initial fusion efficiency directly increases the genetic diversity of the resulting screening pool, enhancing the likelihood of isolating rare, high-affinity B cell clones targeting challenging epitopes.
Table 01: Comparison of PEG-Mediated Chemical Fusion vs. Electrofusion
| Characteristic | PEG-Mediated Chemical Fusion | Electrofusion |
|---|---|---|
| Mechanism | Chemical fusogen (Polyethylene Glycol) induces membrane merger | An electrical field creates pores, inducing fusion |
| Fusion Efficiency | Low | High |
| Cell Viability / Stress | Higher chemical cytotoxicity | Gentler stimulus, low cytotoxicity, and higher viability |
| Control & Reproducibility | Lower controllability | Higher controllability and standardization |
C. Selection, Screening, and Cloning
Once fusion is complete, the subsequent hybridoma technology steps focus on isolating the rare, successfully fused hybridomas.
- Selective Culture: Fused cells are transferred into
selective Hypoxanthine-Aminopterin-Thymidine (HAT) medium.
- Primary Screening: On or around day 10, culture
supernatants are collected and tested for antibody production and specificity,
typically using high-throughput ELISA or flow cytometry.
- Cloning: Positive clones are subjected to multiple rounds
of limiting dilution. This step is vital to ensure that the resultant cell line
is genuinely monoclonal - derived from a single cell, guaranteeing uniform
antibody specificity and consistent production.
Precision Selection: The Molecular Basis of HAT Medium
The entire viability of the hybridoma process relies on the sophisticated biochemical selection mechanism provided by the HAT medium. Addressing what this method is requires an examination of nucleotide synthesis pathways.
The Nucleotide Synthesis Blockade
The key selective agent is Aminopterin. It is a folic acid analog that inhibits the enzyme dihydrofolate reductase, thereby shutting down the de novo pathway required for synthesizing purines and pyrimidines. This blockade forces all cells in culture to rely entirely on the alternative method of nucleotide creation: the salvage pathway.
The Salvage Pathway and HGPRT
The Hypoxanthine and Thymidine (H & T) components are provided to feed this salvage pathway, but their utilization requires specific enzymes, primarily HGPRT (Hypoxanthine-Guanine Phosphoribosyl Transferase). The survival of the cell population is therefore dictated by its HGPRT status combined with its lifespan in culture.
This selection mechanism is an elegant form of synthetic lethality, where only cells possessing both immortality (from the myeloma) and the salvage pathway enzyme (from the B cell) survive by complementing each other's deficiency.
Table 02: Fates of Cell Types in Hypoxanthine-Aminopterin-Thymidine (HAT) Selective Medium
| Cell Type | HGPRT Status | Proliferative Capacity | Fate in HAT Medium | Rationale |
|---|---|---|---|---|
| Unfused B Cells | Present (HGPRT+) | Finite (Mortal) | Die off | Cannot proliferate indefinitely in vitro |
| Unfused Myeloma Cells | Absent (HGPRT−) | Immortal | Die rapidly | Lack of HGPRT prevents salvage pathway utilization when de novo synthesis is blocked |
| Hybridoma Cells | Present (from B cell) | Immortal (from Myeloma) | Survive and proliferate | Inherit HGPRT for salvage pathway survival and indefinite replicative potential |
The necessity for repeated cloning steps via limiting dilution confirms that newly fused hybridomas are susceptible to genetic instability. Even initially successful clones may lose chromosomes over time, potentially impacting consistent antibody expression. This risk highlights why long-term stability requires the modern approach of sequence determination.
Enduring Strengths: Advantages and Application of Hybridoma Technology
The persistent importance of hybridoma technology stems from its unique biological origin, which provides significant advantages over purely in vitro systems.
Biological Advantages of Hybridoma-Derived mAbs
- Authentic In Vivo Affinity Maturation: The initial
immunization cycle compels the B cells to undergo natural somatic hypermutation
and affinity maturation within a living immune system.
- Native Chain Pairing: Unlike synthetic libraries, which
risk random chain association, hybridomas retain the original, native pairing of
the heavy and light chains of the B cell, preserving the authentic structure and
function of the epitope recognition domain (Fab).
- Natural Structure and Function: The antibodies maintain
natural post-translational modifications, including glycosylation patterns,
which are crucial for in vivo functionality, pharmacokinetics, and triggering
effector mechanisms.
- High Yield and Consistency: Once a stable, positive clone
is selected and expanded, the hybridoma line provides an unlimited, continuous
source of the identical, specific antibody.
Critical Applications of Hybridoma Technology
The robust and established nature of this platform makes hybridoma-derived antibodies indispensable across therapeutic and research sectors.
Research and Diagnostics
- Cell Characterization: This technology has
revolutionized immunology by providing specific antibodies used to
define the Cluster of Differentiation (CD) markers, essential for classifying
immune cells, and used globally in techniques like Fluorescence-Activated Cell
Sorting (FACS).
- Clinical Diagnostics: mAbs are used for high-specificity
detection in clinical settings, including serological typing of ABO blood
groups, identification of viral pathogens, and common assays like pregnancy
detection (human chorionic gonadotropin, hCG).
- Pathology: The high sensitivity of these mAbs aids in
immuno-cytological analysis, detecting occult metastases, and determining the
tissue origin of undifferentiated lesions.
Therapeutics
Hybridoma-derived antibodies established the foundation for modern targeted therapies, and are invaluable in the development of numerous FDA-approved treatments for cancer, autoimmune disorders, and infectious diseases.
Downstream Excellence: Hybridoma Technology Purification
A high-quality mAb requires stringent downstream processing (DSP) to remove contaminants present in the crude hybridoma culture supernatant, which contains host cell proteins (HCP), cellular debris, and nucleic acids. Effective hybridoma technology purification is a non-negotiable step to achieve the high purity (typically >90% purity confirmed by SDS-PAGE) necessary for reliable research and clinical application.
The Multi-Step Purification Strategy
01. Capture Step (Affinity Chromatography): The initial step involves affinity chromatography, usually utilizing Protein A or Protein G, which binds specifically to the Fc region of the antibody. This step achieves a significant concentration of the mAb product, capturing the target antibody that typically starts at a low titer (1 to 60 μg/ml) in the culture supernatant.
02. Polishing Steps (Intermediate Chromatography): To remove aggregates, charge variants, and residual HCP/DNA, one or more polishing steps are required.
- Ion Exchange Chromatography (IEX), specifically Anion Exchange (AEX)
followed by Cation Exchange (CEX), is commonly employed.
- Hydrophobic Interaction Chromatography (HIC) may also be used, depending on
the specific impurity profile of the monoclonal antibody product.
03. Final Processing: Techniques such as Ultrafiltration and Diafiltration are employed for final buffer exchange and concentration. These methods enable the removal of smaller macromolecules and can concentrate the monoclonal antibody product significantly, achieving concentrations of more than 25-fold from the initial supernatant.
Advance in Hybridoma Technology: Modernizing a Classic Platform
While the core fusion principle remains, modern technologies have provided a significant advancement in increasing throughput, enhancing specificity, and ensuring long-term stability.
A. Enhanced Screening and Selection Methods
Traditional screening via simple ELISA has been augmented by advanced platforms that enable the selection of higher-quality clones:
- Microfluidics: The use of microfluidic devices allows for
highly precise control over fluid volumes, facilitating the high-throughput,
automated isolation and characterization of individual B cells or hybridomas.
This automation is critical for identifying rare, high-affinity clones that
might be masked in bulk culture systems.
- Kinetic Analysis (BLI): High-throughput screening now
incorporates kinetic analysis using platforms like Bio-Layer Interferometry
(BLI). Unlike ELISA, which only confirms binding, BLI allows researchers to
directly measure dissociation rates. By screening clones based on kinetic
parameters, researchers can prioritize antibodies with superior functional
binding characteristics, accelerating the discovery process.
B. The Transition to Genetic Stability
The most definitive advancement related to this method involves sequencing the antibody genes. Due to the inherent risk of genetic instability and potential chromosome loss in continuously cultured hybridomas, long-term assurance of consistency requires genetic archival.
- Hybridoma Sequencing: The Variable Heavy (VH) and Variable
Light (VL) chain genes of the stabilized hybridoma clone are sequenced.
- Recombinant Expression: Once the sequence (the antibody
blueprint) is obtained, the gene can be cloned into a mammalian expression
vector and produced recombinantly (e.g., in HEK293
or CHO cells). This synergy ensures that the biological specificity
discovered by the hybridoma process is married to the consistency and
scalability of recombinant systems.
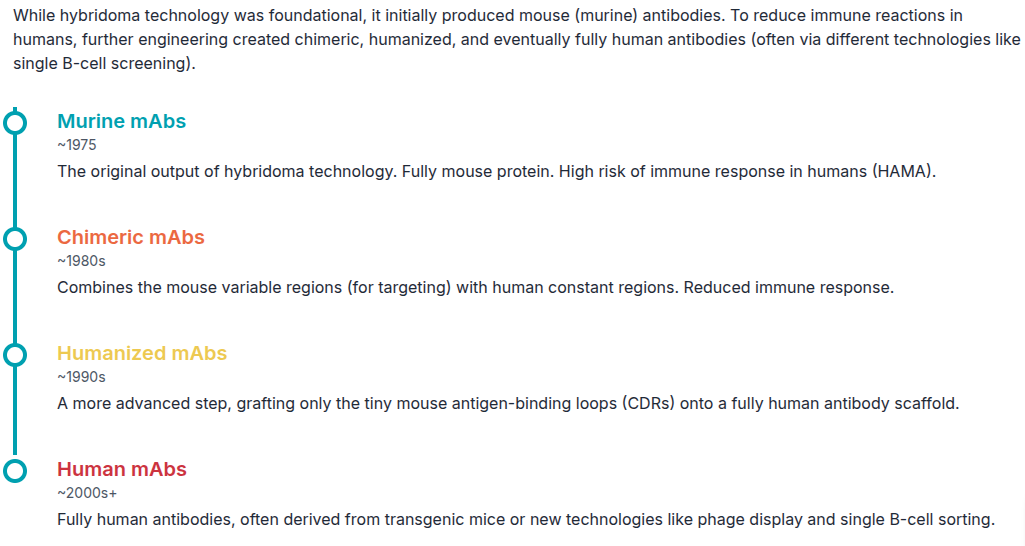
The recombinant format offers crucial long-term benefits: permanent archival as plasmid DNA, reproducible expression from a defined genetic construct, and engineering flexibility, such as isotype switching or humanization, which overcomes the primary drawback of murine-derived hybridomas.
Strategic Comparison: Hybridoma vs. Recombinant Antibody Platforms
Choosing the optimal antibody generation method is a strategic decision for researchers. The strengths of hybridoma and monoclonal antibodies must be weighed against alternative platforms like phage display, which utilize in vitro selection methods.
The classic hybridoma platform carries inherent limitations, including a time-consuming process (often 6 to 8 months for generation and stabilization) and the requirement for animal use. Furthermore, murine-derived antibodies necessitate costly and resource-intensive humanization steps before they can be deployed as therapeutics to avoid immune rejection in humans.
However, this method maintains an edge when the target requires an antibody that has been physiologically optimized. For complex membrane proteins or conformational epitopes, the affinity maturation achieved in vivo often yields superior, functional antibodies compared to in vitro systems, which can suffer from random VH/VL pairing and reduced antigen affinity.
Table 03: Comparative Analysis of Hybridoma vs. Phage Display Antibody Generation
| Feature | Hybridoma Technology | Phage Display / Recombinant |
|---|---|---|
| Origin of Affinity | In vivo affinity maturation (natural immune system) | In vitro library selection (synthetic or naïve) |
| Generation Time | Long (6–8 months average) | Rapid screening |
| Antibody Diversity | Limited by host tolerance / immunogenicity | High |
| Immunogenicity Risk | High (typically murine, requires humanization) | Low (can use fully human libraries) |
| Native Pairing | Preserved (native VH/VL pairing) | Random (risk of suboptimal VH/VL pairing) |
| Long-Term Consistency | Requires sequencing / recombinant stabilization due to genetic drift | High (produced from a defined genetic construct) |
Conclusion: The Indispensable Role of Hybridoma Technology in Antibody Discovery
The invention of hybridoma technology provided the life science community with the first consistent, epitope-specific immune reagents, fundamentally altering the landscape of biotechnology.
The core principles of the exploitation of cellular immortality, coupled with specific immune function, are continually being refined by modern scientific advancement. By integrating electrofusion for high initial yield, kinetic screening for rigorous clone selection, and, crucially, hybridoma sequencing for genetic archival, the process eliminates instability risks and provides a sequence-defined blueprint for scalable, high-purity recombinant production.
AAA Biotech, also known as AAA Bio or AAAbio, is dedicated to supporting high-impact research by providing highly validated antibodies, recombinant proteins, and ELISA kits. Our approach respects the inherent biological specificity derived from proven technologies while applying rigorous downstream processing and sequencing for unparalleled batch-to-batch consistency and technical superiority. This ensures our clients receive the most rigorously tested reagents necessary for success in complex scientific endeavors.
Faq's
Why is the mouse myeloma cell line cultured with 8-Azaguanine before fusion?
Myeloma cells are often cultured in a medium containing 8-Azaguanine to ensure they are fully HGPRT-deficient. This nucleoside analog is incorporated into DNA and is lethal only to HGPRT-positive cells, eliminating any revertant cells that might regain functional HGPRT before the HAT selection step.
What are "feeder cells", and why are they sometimes added to the initial hybridoma culture?
Feeder cells, typically peritoneal macrophages or specific cell lines, are sometimes added to the 96-well plates. They support the growth of low-density hybridomas by secreting growth factors (like IL-6) and providing a conditioned environment to boost the initial survival rate of fragile, newly fused hybridomas.
Besides mice, what other animals can be used for hybridoma production, and what's the challenge?
While mice are the standard, rats and sometimes rabbits are also used. A main challenge is that stable, HGPRT-deficient myeloma cell lines suitable for fusion are less readily available for species other than the mouse
What is the risk associated with the in vivo ascites method of large-scale antibody production?
The in vivo ascites method, involving injecting hybridomas into a mouse peritoneal cavity, yields high antibody concentration. However, the final product carries a risk of viral or host-protein contamination, which necessitates more rigorous and costly purification for therapeutic use.
What determines the specific class (isotype) of the monoclonal antibody produced by the hybridoma?
The isotype (IgG, IgM, etc.) is determined by the B cell fusion partner's state of differentiation and class switching in vivo. The myeloma cell contributes to the immortalization, but the B cell provides the heavy chain constant region gene that dictates the antibody class.