A Comprehensive Guide to ELISA Sensitivity and Specificity
In this Article
- What is Sensitivity and Specificity with Respect to ELISA?
- The Diagnostic Power Curve: ROC Analysis
- Factors Affecting ELISA Sensitivity and Specificity
- ELISA in Food Sensitivity Testing: A Special Issue
- Case Scenarios and Preventative Measures
- The Inter-relations between Clinical Application and Research
All of the products listed in AAA Biotech’s catalog are strictly for research-use only (RUO).
Key Takeaways
- Sensitivity in ELISA is critical for demonstrating the extent of true positives.
- Specificity is used to measure the extent to which it excludes false positives.
- Diagnostic performance is dependent on a trade-off between the two metrics: sensitivity vs specificity.
- High sensitivity eliminates the possibility of a lack of disease detection, whereas high specificity eliminates the possibility of misdiagnosis.
- ELISA tests focused on certain food sensitivities are dependent on sensitivity limits.
- Both of these aspects of a specific ELISA kit must be known in order to perform virtually any research, diagnostics, or therapeutic monitoring.
A small change makes significant differences in diagnostics, which may result in
better patient health outcomes or can complicate problems even further. In the
case of the Enzyme-Linked Immunosorbent Assay (ELISA), accuracy and trust depend
primarily on two performance metrics, i.e., sensitivity and specificity.
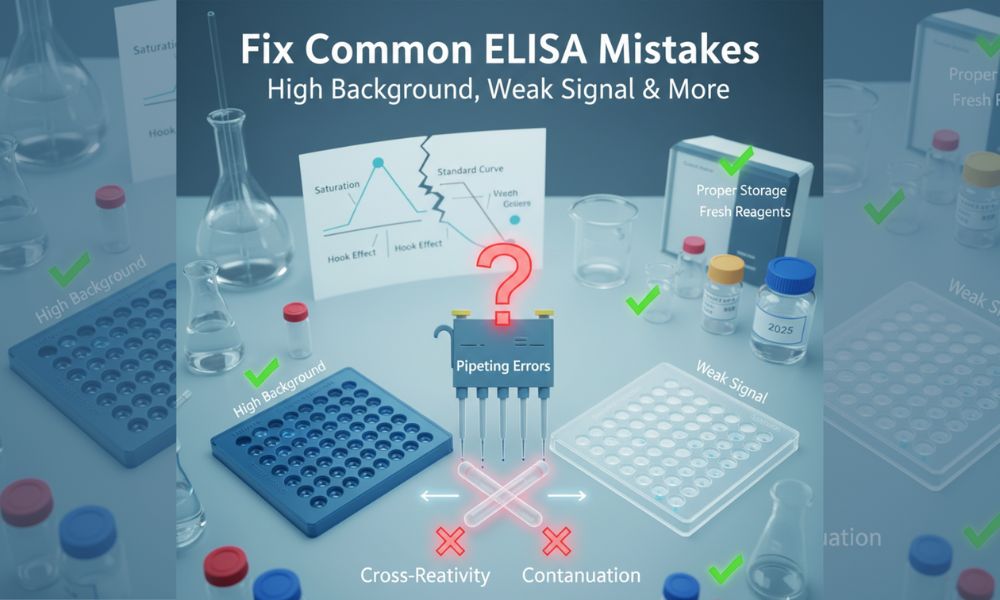
Mistakes in these metrics can result in severe consequences, including false assurances or unnecessary clinical procedures.
As dependence on ELISA tests is growing in the screening of infectious diseases, autoimmunity, and even food sensitivity testing, a keen understanding of an ELISA’s sensitivity vs specificity is not solely important in the technical sense, but it is also imperative in many applications and can be life-affecting.
What is Sensitivity and Specificity with Respect to ELISA?
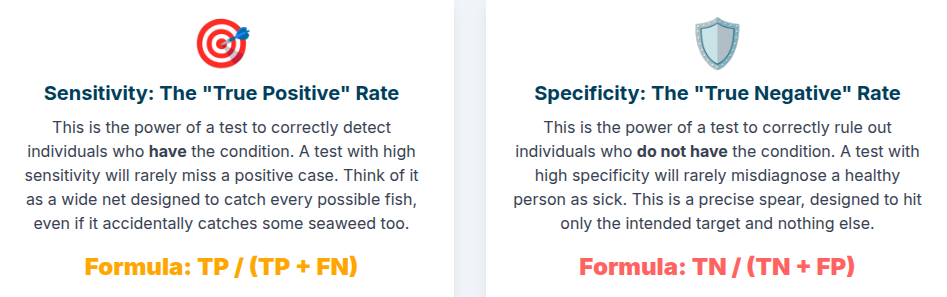
Sensitivity
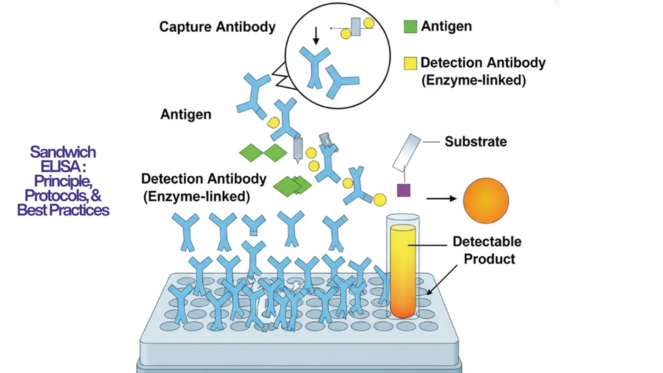
The sensitivity of the assay refers to the ability of accurately detecting samples that possess the target analyte or antibody (true positives).
Formula: Sensitivity = (True Positives/ True Positives + False Negatives) × 100 Sensitivity = (True Positives + False Negatives/ True Positives) ×100
Example: When the ELISA identifies 98 out of 100 HIV
infections, then the sensitivity of the ELISA is 98.
A high-sensitivity ELISA kit is important when one is ruling out life-threatening diseases, whereby the absence of a positive result can potentially have devastating effects.
Specificity
Specificity demonstrates the ELISA capability to correctly “diagnose” samples that lack the target analyte of interest - true negatives.
Formula: Specificity = (True Negatives/True Negatives + False Positives) ×100 Specificity = (True Negatives + False Positives/True Negatives) ×100
Example: If a celiac disease ELISA shows 93 negative results on
100 healthy individuals, the specificity is 93%.
A specific ELISA eliminates “false alarms” in clinical analysis as well as in food sensitivity testing by preventing mislabeling of healthy/normal samples as “diseased”.
Critical Points To Consider for Sensitivity and Specificity
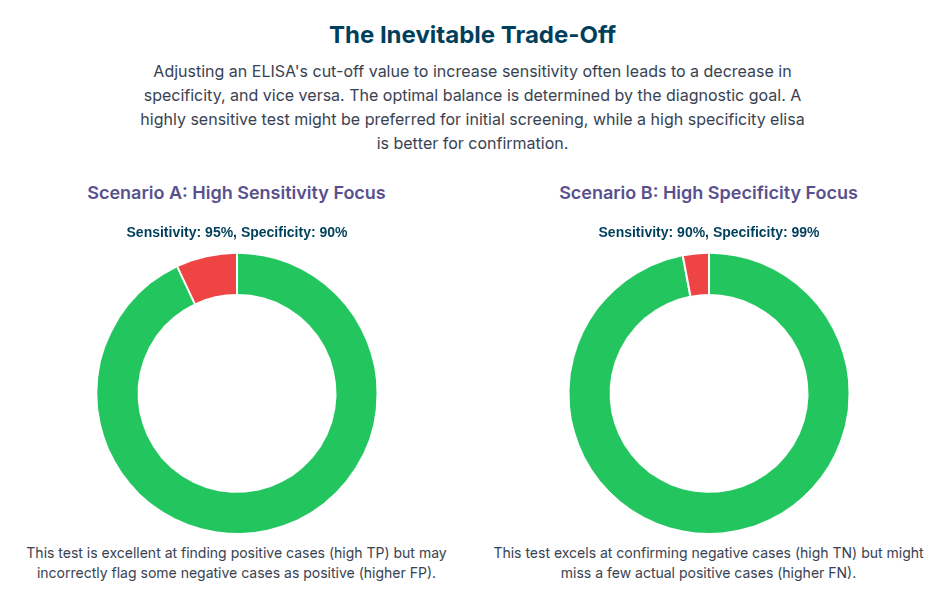
The dilemma is that there are cases when the increase of assay sensitivity leads to a decrease of the specificity and vice versa.
- Enhanced Sensitivity: Sensitive, but it is prone to
cross-reactivity as well as false positives.
- Increased Specificity: Only the target molecule is recognized, but it cannot give a result for samples containing a low-abundance of the target analyte.
Balance is desired because the accuracy of ELISA tests is assessed on both
measures.
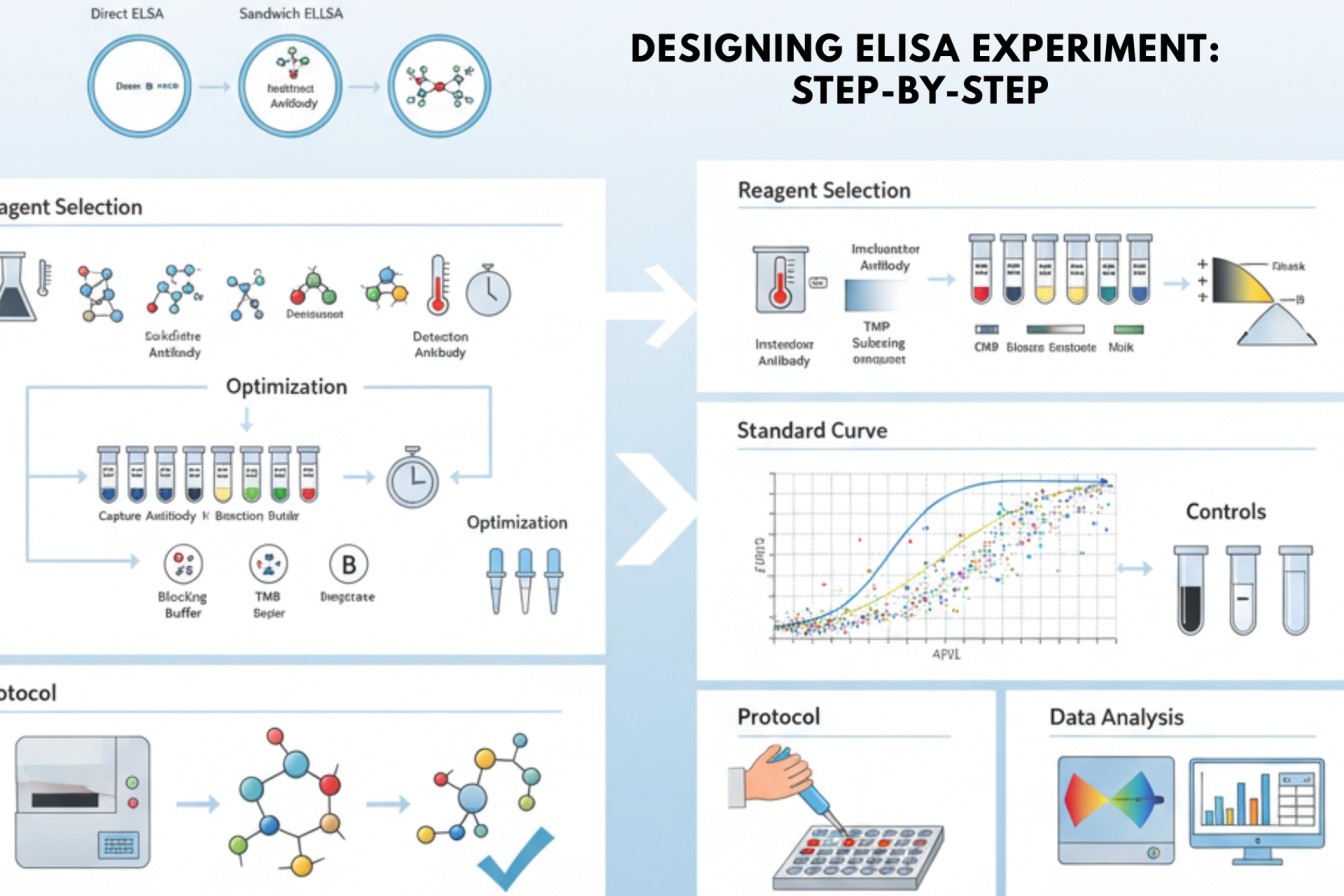
The Diagnostic Power Curve: ROC Analysis
The utility and credibility of an ELISA are represented as Receiver Operating
Characteristic (ROC) curves.
An ideal test will have the specificity and sensitivity, and will have an area under the ROC curve (AUC) of 1.0. The AUC of most ELISAs is typically around 0.9, indicating a high degree of accuracy, but with potential trade-offs.
ELISA test reliability is confirmed by researchers using raw measures that include ROC interpretations and cut-off optimization.
Factors Affecting ELISA Sensitivity and Specificity
Critical factors affecting these metrics include:
Antibody Quality
- Cross-reactivity may cause polyclonal antibodies to be more sensitive but less specific.
- Specificity is increased by the use of monoclonal antibodies, which bind to
one single epitope.
Interference with Samples
- A low purity of the analyte can lower the accuracy of the ELISA test.
- Autoantibodies, as in the case of lupus ANA
testing, can interfere and distort reliability.
Kit Design
A frequently used ELISA test principle of “signal amplification” in a high-sensitivity ELISA is tyramide or chemiluminescence detection, which all but guarantees the detection of trace analytes.
Sample Matrix
ELISA test reliability is influenced by the composition of the sample (ie. serum vs plasma vs saliva), since different sample types will invariably have different potentially interfering proteins.
ELISA in Food Sensitivity Testing: A Special Issue
When it comes to testing for food sensitivity, these two competing metrics can
lead to complications, making balancing assay responsiveness and specificity of
greater importance than usual.
In this case, the ELISA assay sensitivity needs to identify the presence of trace allergens (e.g., gluten, peanut proteins), which are typically present in parts-per-million (PPM) concentrations. Meanwhile, false alarms and unjustified dietary restrictions are potential outcomes due to the possible cross-detection of harmless food components in the sample being tested.
Case Scenarios and Preventative Measures
High Sensitivity Priority
- Infectious disease (HIV, COVID-19 antibodies) screening:
There should not be a single positive sample missed.
- Strategy: Decrease the cut-off, apply a signal-enhanced
chemistry luminescence system.
High Specificity Priority
- Confirmatory autoimmunity or allergen screening: This is to
prevent falsely diagnosing somebody with dietary restrictions that they are not
able to avoid.
- Strategy: Multiple antigen verification, use monoclonal
antibodies.
The Inter-relations between Clinical Application and Research
The dynamic relationship between clinical application and research, with respect to ELISA, involves:
01. Clinical diagnostics: Balance between the two major ELISA metrics frequently determines patient treatment methods.
02. Therapeutic monitoring: It is necessary to identify, for instance, drug levels, relevant to both aspects with high precision.
03. Food safety testing: It is important to optimize these metrics to avoid acting upon on a potentially false alarm, such as with gluten-free labeling (as it has a high ELISA detection limit).
Lastly, regulatory acceptance and trust, in addition to that of the consumer, highly depend on the accurate development and balance of an ELISA test’s sensitivity and specificity.
Conclusion
ELISA has been an effective tool in both diagnostics and research. However, it can only exercise its robust power when its outcomes are interpreted based on a holistic knowledge of the individual ELISA’s sensitivity and specificity.
It has been observed and accepted that the performance of any test is not going to be simple and applicable to every experimental model, as sample compositions can be quite complicated, and the populations that the samples are sourced from can vary widely
ELISA test accuracy and reliability are not simply numbers on a page that should be ignored or taken for granted. They are the bases of credible science and effective decision-making.
Faq's
What is the difference between the ELISA sensitivity and detection limit?
The lowest measurable detectable analyte concentration is known as the detection limit, whereas sensitivity is a measure of the correct rate of actual positives.
Is it possible to enhance ELISA specificity and sensitivity at the same time?
Trade-offs are typically present. Nevertheless, better antibody engineering, recombinant antigen design and efficient signal detection systems can certainly help maximize the two.
What is the reason that ELISAs concerning food tend to focus on high sensitivity?
Due to the ability of trace allergens to cause a reaction, it is important to make sure that even microgram-level detections are not missed, even at the cost of a few false positives.
Is it sensitivity or specificity that is more important?
It depends; in the case of early screening, sensitivity is a must. Specificity is more significant for confirmatory diagnosis.
In what ways is the reliability of an ELISA test determined?
Through replication and validation on a large population of samples and ROC curve analysis to optimize the cut-offs.